According to the Center for Disease Control (CDC), public health is defined as “the science of protecting and improving the health of people and their communities. On the other hand, public health is concerned with protecting and evaluating the health of entire populations.” These populations vary in size and density, ranging from small, rural neighborhoods to an entire country or continent.
In seeking to understand the unique aspects of a community’s relationship to health, researchers have tied seemingly isolated data patterns to larger trends across demographic divides. Here, stark disparities between groups reveal themselves, illustrating chronic health inequalities stemming from inequity.
Health inequality vs. health inequity
Health inequalities serve as a canary in the coal mine by pointing to deep-rooted inequities within communities, urging public health activists, researchers, policy makers, and healthcare providers to take a closer look.
Before going any further, it is important to differentiate two terms that are often used interchangeably, despite having two distinct meanings: health inequality vs. health inequity. According to the National Library of Medicine, health inequality generally refers to differences in the health of individuals or groups. It is the measurable aspects of health that vary from individual to individual, or group to group. Health inequity, however, is a specific type of health inequality that denotes an unjust difference in health.
SDoH are a huge factor in health
Also referred to as SDoH, the Office of Disease Prevention defines social determinants of health as “the conditions in the environments where people are born, live, work, play, worship, and age that affect a wide range of health, functioning, and quality-of-life outcomes and risks.”
Social determinants of health are grouped into five key categories - economic stability, education access and quality, social and community context, neighborhood and built environment, and health care and quality.

Believe it or not, these five categories determine more about a person’s potential health outcomes than their genetics. Sound far-fetched?
Consider the role of the social community to which a person belongs. While this may sound farther removed from wellness than DNA, having a sense of belonging and social support can be the difference between life and death. Take, for example, the relationship between loneliness and mortality. Loneliness increases the risk of death by a shocking 26%. A sense of isolation or feeling disconnected from others is prevalent in 63% of those experiencing depression or clinical anxiety, two disorders tied to shortened lifespans, and chronic illness.
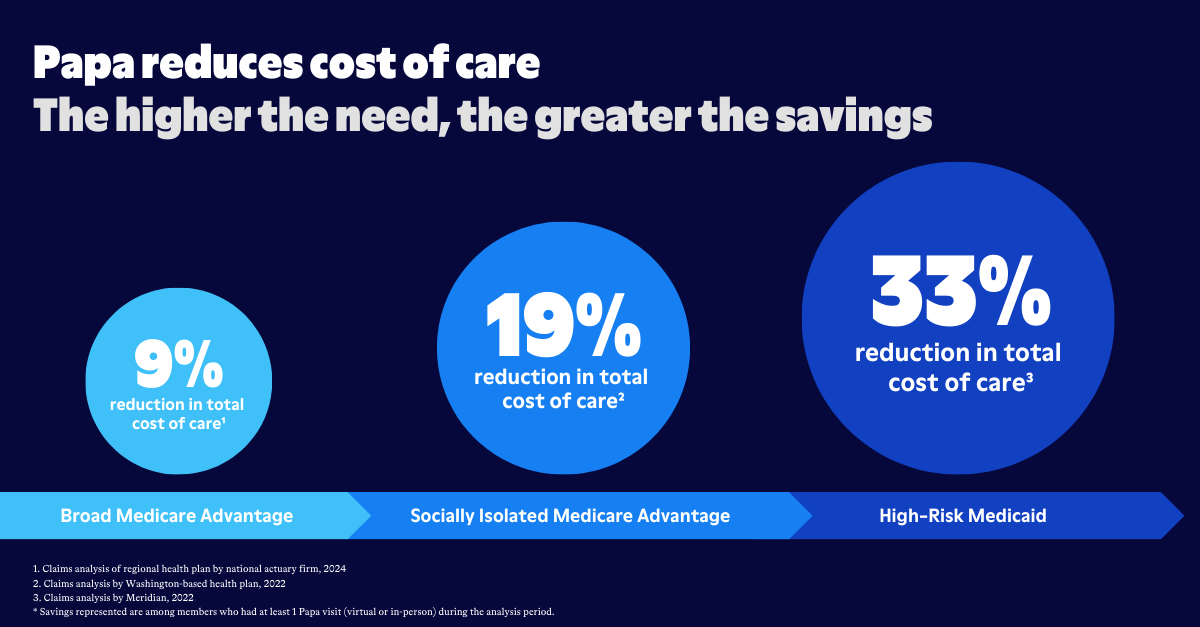
In addition to living with mental health inequalities, those without a strong sense of social support also face increased risk of physical ailments. When people don’t have friends and family around, they often ignore or don’t notice serious health concerns. Bad eating habits, lack of exercise, and failure to attend regular health visits all increase the prevalence of serious illness, and with that, more trips to the emergency room.
In the case of loneliness, young adults and mothers are disproportionately affected. Recent data shows that 36% of all Americans—including 61% of young adults and 51% of mothers with young children—feel serious loneliness. This number—which has increased 13% since the pandemic—indicates a serious health care crisis.
As for the physical implications of being disconnected from your community, the elderly take on serious safety risks. Falls alone can be disastrous for aging adults, and when these take place without anyone else around, they become infinitely more dangerous. More than 800,000 people are hospitalized every year from falls, costing the healthcare system more than $500 billion annually.
Between emergency visits, hospitalizations, depression, and treatment, social disconnection weighs on mental, emotional, and physical health. It also threatens economic stability. Another SDoH, economic stability, comes with its own side effects, and tells a tale of racial inequity.
To improve public health and prevent further disparity, it is critical that healthcare organizations address how interconnected social determinants of health are, and attack these issues right at the root cause.
Prevention is key to individual…and public health
We recognize the herculean task that improving public health it is. Public health requires attention and dedication from an array of governmental, private, and citizen-led bodies. From policy to infrastructure to advocacy, we understand that efforts to alleviate health inequity must be multi-prong and unified.
At the same time, we’ve seen that the smallest change can make a huge difference in the lives of individuals. When healthcare takes the lead and seeks out solutions geared toward prevention, entire communities reap the benefits. Given what we know about the social determinants of health, health care providers can see what people need, and build a roadmap toward greater public health.
In our guide, SDoH Data Decoded, Papa delves deeper into each SDoH, the issues faced there within, and offers solutions in the form of people. Through one-on-one connection and support, we’re working to change the way people live, for the better.