Behavioral health issues among older adults, including anxiety, cognitive impairment, and mood disorders, have always been major drivers of Medicare spending in particular. But now those conditions are more prevalent than ever—and experts say the pandemic is largely to blame.
While behavioral health issues have always been impactful for Medicare Advantage plans and their members, this impact has only grown worse over the last couple of years due to the pandemic.
Health plan administrators are well aware that people of all ages with mental health disorders have longer hospital stays, incur higher outpatient costs, and seek care for other medical ailments more than the population at large. For many older adults, these issues are often compounded by pre-existing chronic diseases and conditions like social isolation and loneliness.
An older adult with heart disease or cancer may be more susceptible to developing depression, for example, and if they happen to be socially isolated and living at home alone, their condition could easily go undiagnosed.
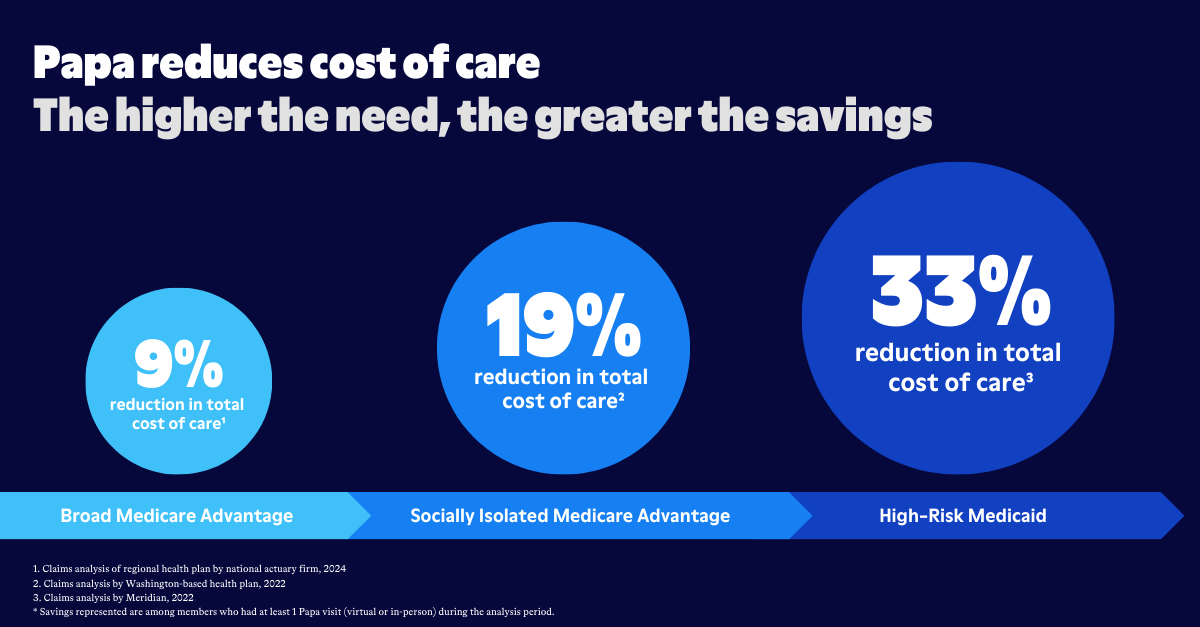
For Medicare Advantage plans, the bottom line is that behavioral health disorders lead to worse health outcomes and increased health care costs, especially in the older adult population. The challenge for plans that hope to turn this trend around: finding a way to identify and treat these conditions early so associated health care spending can be better controlled.

Disorders driving health care spending
The question of how to address behavioral health challenges among older adults is nothing new for health who are focused on improving member experience while reducing costs.
One study published by the American Medical Association in March 2020—just before the pandemic began in the United States—revealed that while about 4 percent of Medicare spending was devoted to mental health services for older adults, that figure more than tripled when one considered the impact that behavioral health disorders have on other medical conditions.
In total, the researchers found, nearly 13% of total Medicare spending was associated with treating behavioral health disorders and related conditions. “The presence of a mental illness can profoundly affect the ability of patients and health systems to manage other chronic medical conditions," the study noted. These conditions ranged from diabetes, to heart failure and even chronic obstructive pulmonary disease, the study noted. “In turn, increased risk for and poor management of chronic conditions could lead to worse health outcomes and greater use of health care services.”
If that conclusion was true in early 2020, researchers say it’s even more true today.
In a National Poll on Healthy Aging conducted by the University of Michigan, researchers found the pandemic had created “unprecedented challenges for older adults that can negatively affect mental health.” The majority of older adults who participated in the survey reported they were in good mental health, but one in five said they struggled with at least one mental health disorder, and 18% said their mental health had worsened since the pandemic began.
Behavioral health disorders
Behavioral health (mental health) disorders affect how people feel, think, and behave. They may include:
- Anxiety disorders like panic disorder, obsessive-compulsive disorder, and phobias
- Mood disorders like major depression
- Eating disorders
- Personality disorders
- Post-traumatic stress disorder
- Psychotic disorders like schizophrenia and bipolar disease
Companion care: Closing gaps in mental health treatment
When older adults who are experiencing behavioral health challenges seek professional help for their conditions, they can usually be treated easily and effectively with medications and other interventions. According to the Michigan survey, however, only half of those who said they were struggling with such conditions during the pandemic said they’d gone to a mental health professional for help. And other studies have found that Medicare beneficiaries, have reduced utilization of mental health services since the pandemic began.

So what can Medicare Advantage plans do to help their members get the behavioral health help that they need? One increasingly popular solution is to offer companion care as a supplemental benefit.
Companion care involves having trained and vetted assistants spend time one on one with your members in their homes and in their communities. These professional companions know how to recognize behavioral health disorders, and they’re well versed in the health care services that are available for people with behavioral health conditions. In their daily visits with the older adults they see, they help them with everything from transportation to the pharmacy to scheduling appointments with their health care providers, and most of all, companion caregivers often become close, trusted friends.
They’re not just there to get a sense of the member’s state of mental health, but if problems do arise, they’re ready to ensure that health care is just a phone call away.